Applications of Cytokines and Growth Factors in Cancer Research
Understanding cancer has been similar to the parable of the blind men describing an elephant based on touch. Depending on what part of the elephant each blind man touched, one would get a different description of the beast. So it is with cancer. The causes of cancer have at various times been described as a series of mutations, viral infections, failures of apoptosis, and failures of the immune system. Cancer is all of these and more; however, simply put, cancer is cells out of control. The question is, how do these cells get out of control?
Normal cells of multicellular organisms are constantly signaling to one another via molecules called growth factors and cytokines. The signals released by growth factors and cytokines can tell individual cells whether to divide or not. Cytokines also signal the immune system, triggering white blood cells to mount coordinated attacks on invading bacteria, viruses, and fungi.
One of the first hints of a connection between cancer and growth factors came from the observation that normal cells in culture required serum for proliferation, while cancer cells had a markedly reduced requirement for serum. It is now known that among other things, serum provided growth factors needed to signal cells to undergo mitosis. The next clues came from several oncogenes, mutations found in cancer cells, observed to behave either in a manner similar to or directly related to growth factors and their receptors. For example, the sis oncogene product was found to be closely related to the Chain B of plateletderived growth factor (PDGF), and like the PGDF family, the sis oncogene and the simian sarcoma virus that harbors it, only affect mesenchymal cells like fibroblasts.
Similarly, the oncogene erbB can be related to the Epidermal Growth Factor Receptor (EGFR) family. In the case of erbB, the gene product was found to be a truncated version of the EGF receptor, resulting in affected cells growing and dividing even when little or no growth factor was present. In several cases mutations have resulted in overexpression of an EGF receptor, as in the case of the oncogenes ERbB2, HER2, and Neu. The overexpressed receptor constantly signals the cell to divide and grow even when little or no growth factor is present. The overexpression of the EGFR family of receptors is present in a third of all human cancers and has served as targets for several cancer drugs including Erbitux®, Herceptin®, Vectibix™, and Tarceva®.
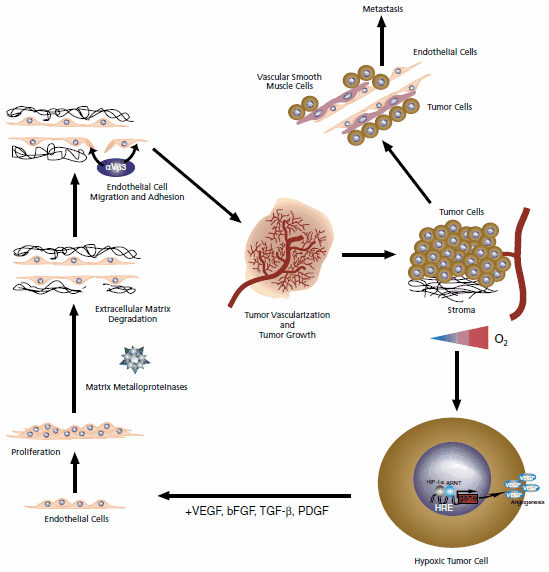
Figure 1.Events leading to angiogenesis and metastasis.
While cancers cells can multiply out of control, they cannot form tumors without a sufficient blood supply. Cancer cells often overexpress the Vascular Epithelial Growth (VEGF) family of growth factors as well as PDGF, TGF-a, and others to promote the development of blood vessels. The constant expression of these growth factors results in abnormal, inherently leaky, blood vessels. The increased porosity of leaky vessels impairs blood flow and slows the perfusion of cancer drugs in tumors. Ironically, the structure of these abnormal vessels has also been exploited for drug delivery strategies. The larger pores allow liposomes containing therapeutic drugs and large drug complexes composed of polyglutamic acid to enter tumor tissues more freely. The normal, relatively non-porous, blood vessels protect non-cancerous tissues from the cytotoxicity of cancer drugs when these drug delivery strategies are employed.
Given tumors require vascularization for growth, blocking blood vessel formation has become a major strategy to fight cancer. An anti-VEGF monoclonal antibody called Avastin® has been shown to block blood vessel formation and maintenance in tumors, slowing the progression of cancer. In the long term, unfortunately, cancer cells often adapt and use other growth factor families for recruitment of new blood vessels. These secondary pathways are also being investigated as new drug targets for cancer therapeutics.
As mentioned earlier, another aspect of cancer is a failure of the immune system to recognize tumor specific antigens. Cytokines behave similarly to growth factors, causing cells to grow and divide; however, they are the predominant cellular signals of the immune system and have other actions such as attaching (chemotaxis) white blood cells to the site of an infection. Interestingly, it has been shown cancer cells signal suppressor T cells to protect them from killer T cells against unique tumor antigens. The mechanism of recruitment is not fully understood but TGF-b and interleukin 10 (IL-10) have been implicated in regulatory T cell function. While some cytokines play a role in suppressing the immune system, others such as IL-2 play a role in activating the immune system. One of the strategies in battling cancer has been to exploit the ability of interleukin-2 (IL-2) to heighten the immune response. IL-2 has been shown to cause complete remission in 6% of patients with renal cancer.
As stated earlier cytokines and growth factor families are an important aspect of cancer research. The connection of growth factor families and oncogenes has lead to a better understanding of carcinogenesis as well as providing new targets for chemotherapy. Several cancer therapies, which target growth factor receptors, have now been FDA approved and more are in the pipeline. So far none of these therapies have been completely effective, but all have been shown to improve the survival of cancer patients.
References
如要继续阅读,请登录或创建帐户。
暂无帐户?